September 5, 2024 — A new collaborative study led by researchers at the Hebrew University of Jerusalem has revealed crucial insights into the cellular events leading to the onset and progression of Alzheimer’s disease (AD), as well as cellular dynamics that contribute to brain aging.
According to the study published in Nature, the international research team mapped 1.65 million cells from 437 aging brains. They uncovered distinct paths of cellular change in the aging brains, with one leading to Alzheimer’s disease and another to an alternative form of brain aging, providing a foundation for personalized therapeutic development.
“The insights from this research provide a fresh understanding of how Alzheimer’s disease develops, from the very early stages, which was not possible to measure without our large dataset and unique algorithmic approach,” said Dr. Naomi Habib of the Hebrew University Edmond and Lily Safra Center for Brain Sciences. “We have paved the way to early identification of people at risk of Alzheimer’s disease and for targeted treatments of each form of brain aging to promote healthy aging.”
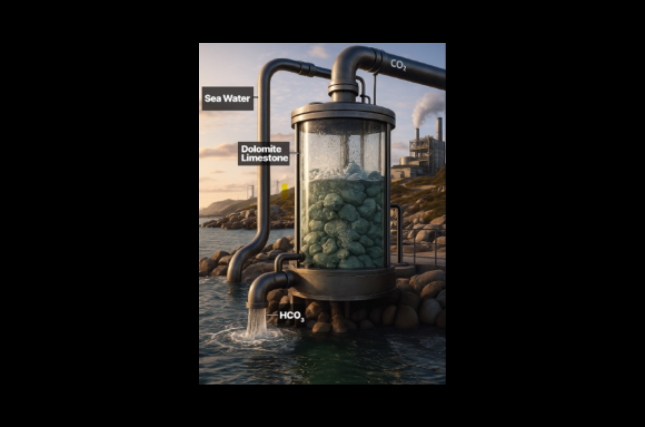
Alzheimer’s disease is characterized by hallmark brain pathologies, with the classical Amyloid theory of AD describing the cascade of events thought to follow the progression of the disease – starting with the accumulation of amyloid-β plaques, which then lead to the accumulation of toxic neurofilament tangles, eventually leading to substantial neuronal damage and symptoms of clinical dementia. Glial cells, such as microglia and astrocytes, are supportive cells that are critical for the correct function of the brain and of neuronal cells, yet have only been recently suggested to take part in the cascade leading to Alzheimer’s disease.
The study uncovered two different subsets of microglial cells, both linked to altered lipid metabolism. The team predicted one that drives amyloid-β plaque buildup, the initial hallmark pathology of Alzheimer’s disease, while the other is predicted to drive the later accumulation of neurofilament tangles. The team also highlighted a group of astrocyte cells that directly influence cognitive decline, shedding more light on the complex interactions between different brain cells in the progression of Alzheimer’s disease and highlight the key role that glial cells are taking in the progression of the disease. The researchers predict that these cellular changes, that start early—before any clinical signs of dementia—are actively determining the fate of the aging brain and the progression of the disease.
Mapping Brain Aging: A Closer Look at Brain Cells
This study took an in-depth approach to map the brain’s cellular environment, analyzing a unique dataset of 1.65 million single-nucleus RNA sequencing profiles from the prefrontal cortex of 437 older adults in the ROSMAP cohort at Rush University in Chicago, IL. With this large dataset, researchers were able to pinpoint specific glial and neuronal cell groups linked to traits related to Alzheimer’s disease (AD). Moreover, the study zeroed in on the complex dynamics within the brain cells along the progression of aging and disease, using a new algorithm called BEYOND to model these dynamics.
The findings lay a cellular foundation for understanding the different paths leading to Alzheimer’s. This knowledge is vital for developing personalized treatments that can act at the cellular level, potentially changing the course of the disease.
The research paper titled “Cellular communities reveal trajectories of brain aging and Alzheimer’s disease” is now available in Nature and can be accessed here.
Nature. 2024. doi: 10.1038/s41586-024-07871-6
Researchers:
Gilad Sahar Green1, Masashi Fujita2, Hyun-Sik Yang3,4, Mariko Taga2, Anael Cain1, Cristin McCabe3, Natacha Comandante-Lou2, Charles C. White4, Anna K. Schmidtner1, Lu Zeng2, Alina Sigalov2, Yangling Wang6, Aviv Regev3,8, Hans-Ulrich Klein2, Vilas Menon2, David A. Bennett6, Naomi Habib1, Philip L. De Jager2,4
Institution:
- Edmond & Lily Safra Center for Brain Sciences, The Hebrew University of Jerusalem
- Center for Translational & Computational Neuroimmunology, Department of Neurology and Taub Institute for Research on Alzheimer’s Disease and the Aging Brain, Columbia University Irving Medical Center
- Harvard Medical School, Boston, MA; Center for Alzheimer Research and Treatment, Department of Neurology, Brigham and Women’s Hospital, Boston
- Broad Institute of MIT and Harvard
- Klarman Cell Observatory, Broad Institute of MIT and Harvard
- Rush Alzheimer’s Disease Center, Rush University Medical Center